Patients
-
- Angiography
- Angioplasty and Stenting
- Aortic Aneurysms
- Biliary Drainage and Stenting
- Carotid Artery Stenting
- Central Venous Access
- Colonic Stenting
- Fibroids
- Gastrointestinal Haemorrhage
- Gastrostomy
- Hepatic Malignancies
- Kidney Tumour Ablation
- Minimally Invasive Treatments for Vascular Disease
- Nephrostomy
- Oesophageal Stents
- Pelvic Venous Congestion Syndrome
- Percutaneous Nephrolithotomy
- Prostate Artery Embolisation PAE
- Pulmonary Arteriovenous Malformations
- PAE Patient Information Leaflet
- Ureteric Stenting
- Varicoceles
- Varicose Veins
- Vascular Malformations
- Vertebral Compression Fractures
- Vertebroplasty and Kyphoplasty
Varicoceles
Webpages based on original contribution by Dr Davis Thomas (Interventional Radiologist, Northampton General Hospital) and Dr Dhruv Patel (Radiology Department, St Georges Hospital)
What is a Varicocoele?
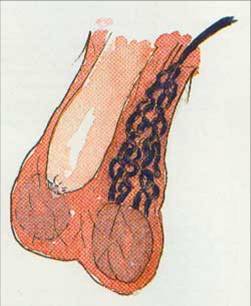
A varicocoele is the swelling in the scrotum caused by a collection of abnormally large bloods vessels (veins) in the scrotum. This is due to dilatation of the testicular vein which drains the scrotum and testicle and is a form of varicose vein. They are often described as feeling like “a bag of worms”.

 A varicocele occurs in approximately 1 in 8 men and it is usually first noticed between the ages of 12 to 28. The incidence is noted to be higher in infertile couples, often up to 30%.
A varicocele occurs in approximately 1 in 8 men and it is usually first noticed between the ages of 12 to 28. The incidence is noted to be higher in infertile couples, often up to 30%.
They usually occur on the left hand side but can occur on both sides of the scrotum. They occur more frequently on the left side as a result of the differing anatomy of the veins from which varicoceles result on the left hand side of the body compared to the right.
Usually veins have a one-way valve that allows blood to flow from an organ to the heart and not the reverse. However, sometimes these valves fail and in this case, this results in blood pooling around the testicle in the scrotum due to gravity. This eventually leads to the veins enlarging and forming a varicocoele.
What are the symptoms?
If they are small, which varicoceles normally are, they produce very few symptoms. In the minority of those affected, one can experience a “heavy” sensation or a feeling of a lump within the scrotum. As the varicocele is caused by pooling of blood within blood vessels, their appearances are often dependent on gravity. They may become more prominent on standing up and at the end of the day. Others may have symptoms such as pain or discomfort, small testicles or infertility.
Pain
This is often described as a discomfort or aching sensation particularly by the end of the day when the person has been standing or sitting for a long period of time. This is thought to be due to increasing pressure in the varicocoele due to increased blood pooling.
Infertility
There is an association between infertility and varicocoeles. Most men with varicocoeles are not infertile. However, if you have a varicocoele, then there an increased chance of infertility. Among infertile couples, the incidence of a varicocoele is about 30%. It is thought that the increased blood flow around the scrotum is responsible for raising the temperature in the testicles and results in defective sperm formation. Varicocoeles may cause decreased sperm count, decreased motility of sperm, or an increase in the number of deformed sperm.
Testicular atrophy
Another symptom of varicocoeles is the shrinkage of the testicles, also known as atrophy. This may recover following treatment.
How are they diagnosed?
The diagnosis of a varicocoele is fairly simple by clinical examination and by using an ultrasound scan. Using colour-flow (Duplex scanning), the veins are easily demonstrated. The ultrasound scan is painless and has no harmful side effects. It can be used at the same time to examine the kidney as very occasionally an abnormal kidney can be the cause for a varicocoele. A venogram may also be performed occasionally, which involves injecting a special dye into the veins to show them up on x-rays. Magnetic resonance scans can also be used but are expensive and rarely required

Varicoeles are usually on the left side. The testicle is sometimes smaller in size.
On examination, they feel like a “bag of worms” which is due to the palpable veins. The size often increases on doing the valsalva manoeuvre (by holding one’s breath and straining down or by blowing hard against a closed mouth and nostrils). On lying down, the varicoele often reduces in size.
Why do they occur?
The vast majority of varicoceles occur as a result of defective valves within the veins themselves. Normally, there are multiple valves in the scrotal veins which only open in one direction and therefore only allow the passage of blood in one direction. In most patients with varicoceles, these valves are defective leading to pooling of venous blood in the veins.
In very rare occasions, the varicocele may develop as a result of a growth in the abdomen causing high pressures on the veins. This situation is an uncommon one and tends to only occur in patients above the age of 45. However, when a doctor finds a varicocele on an ultrasound scan, don’t be surprised or alarmed if he/she also scans your kidneys at the same time.
Can they be serious?
Varicoceles generally cause no serious physical side-effects. The main concern related to varicoceles is male infertility. Variococeles have been associated with lower sperm counts and a lower level of sperm function than normal. They occur in approximately 25 to 40% of males with infertility. Studies are yet to fully explain why they cause reduced fertility, but the most popular theory is that they raise the temperature of the scrotum and thus reduce normal sperm number and function. They may also, if very large, lead to a reduction in the volume of the testis next to it - this is known as testicular atrophy.
In addition, as mentioned before, the sudden appearance of a varicocele in an older patient may relate to an abnormality of the kidney. Such an abnormality would be discovered by an ultrasound scan or a CT scan.
Should varicoceles be treated?
Varicoceles often need no treatment. If you are not suffering from any symptoms or problems as a result of them, then usual medical advice is to leave the varicocele alone. Occasionally, you may experience mild intermittent discomfort from the varicocele, which may be helped by using more supportive underpants, rather than boxer shorts.
If you have a varicocele and you are having trouble with fertility, you may be advised to have the varicocele treated. Current evidence shows that whilst markers of semen quality such as sperm counts and motility do improve following varicocele treatment, overall fertility rates do not improve.
If a varicocele is causing you significant discomfort which is enough to interfere with your daily activities, then treatment is also advised. This can be in a number of forms.
Drugs: There are no medicines available to actually cause a varicocele to shrink or disappear. Any medicines used would be for pain relief only.
Surgery: Surgery is an option for the treatment of varicoceles. This can be performed via a variety of incisions, and can even be performed by laparoscopic “keyhole” surgery. The principle of surgery is that it involved tying off the veins leading to the varicocele. Removal of the varicocele can also be undertaken, but this is to be avoided in all but the smallest of varicoceles and can be a difficult procedure for the surgeon.
Unfortunately, all operations for varicocele repair can be technically challenging due to the large number of veins involved. Furthermore, the operation usually requires a general anaesthetic and there is a recurrence rate of around 10 to 20%.
Radiology: Radiologists are doctors trained in the use of x-ray equipment, and in the interpretation of the images produced. It is now possible to use x-rays to provide images of the veins leading from the varicoceles, and then use these images to inject substances into the veins in order to shrink the varicocele. This technique is called Varicocele Embolisation, and is performed by doctors called Interventional Radiologists.
How do I prepare for a varicocele embolisation?
You may or may not be given a bed in the hospital, depending on local hospital preferences and your level of fitness.
You will be given a time for the procedure and will be asked not to eat for 4 hours beforehand. You will be able to drink water however.
Upon arriving in the Radiology department, you will be asked to change into a hospital gown, if not already done so.
Let the radiologist and nursing staff know if you have any major health problems, allergies, kidney problems or are diabetic.
The staff involved will ask you to confirm your name and date of birth – don’t be alarmed by this or feel it is a sign of poor organisation; it’s a mandatory requirement that we do this for every case.
How is varicocele embolisation performed?
You will have an opportunity to discuss treatment methods with your surgeon and the radiologist prior to an attempt at embolisation and you will also be asked to sign a consent form indicating you are willing for the procedure to take place.. The procedure is carried out in the x-ray department and utilises “live” x-rays and real-time imaging.

Varicocele embolisation involves the patient lying down on an x-ray table, generally on one’s back. An ultrasound scan examining the scrotum may be performed prior to any x-rays being used. The doctor or nurse may put a needle into a vein in your arm in order to give you any necessary painkillers or sedation but these are rarely required.
Generally, the doctors and nurse will also be monitoring your pulse rate, breathing rate and blood pressure using special equipment.
Interventional radiologists can perform varicocele embolisation via a variety of routes, but the two most common are via the veins in the groin or the neck. Depending on which site has been chosen, antiseptic skin cleaning solution will be applied to the skin and then sterile drapes attached around the area in question. There may also be a need to shave some hair from the area. The doctor will then use local anaesthetic to numb the skin and deeper tissues. This is often the part of the procedure which causes the most discomfort, but after a minute or so you will not be able to feel pain. You still however will feel touching and prodding so don’t be alarmed by this. If you do feel pain, let your doctor or nurse know so that they might administer more painkiller and/or anaesthetic. Most patients find that the initial insertion of the needle and the local anaesthetic fluid is the most painful part of the procedure, but that after this stage, no significant pain is experienced.
Once the radiologist is happy that the area has been anaesthetised, they will place a larger needle in the large vein at the site of their puncture. You may be asked to perform some rather odd breathing manoeuvres to distend the vein and make it easier to hit with the needle. This needle will be used to introduce a variety of thin-bore guide-wires and tubes called catheters into the veins leading from the varicocele. This will be all be guided using x-rays and dye injected to the veins to provide images. Once in the correct position, the radiologist can block the veins from the varicocele by injecting either metal coils or less commonly, a glue-type material called sodium tetradecyl sulfate (STS). These materials cause the blood in the veins to clot, and blocks them.

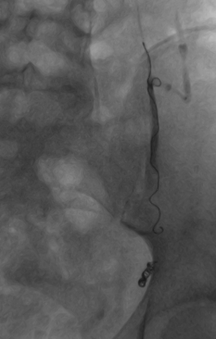
Left sided varicocoele being treated by placement of coils

Embolisation coil
The successful blockage of these veins will be checked by the radiologist by ensuring that no dye injected down the catheter and into the veins, passes beyond the coils/STS. Once the doctor is satisfied with the outcome, the tubes and wires will be removed and the doctor will press down on the vein for several minutes to ensure that there is no bruising or bleeding from the needle puncture site.
Are there any risks?
The overall risk rate is very low. Although results vary from centre to centre, in experienced operators hands, the overall success rate is approximately 90 to 95%, with a rate of over 90% in dealing with pain attributed to a varicocele.
There may be some bruising at the site of the needle puncture into the vein. This will usually resolve after a week. If the bruising if especially uncomfortable or if the surrounding skin becomes red and inflamed, it may be a sign of infection and you may require treatment with a short course of antibiotics. This is an extremely rare complication however.
There is a risk of an allergic reaction to the dye used in the procedure. All the staff are trained in dealing with such a situation and medicines used to treat the reaction is kept within the X-ray rooms themselves.
There is a risk of recurrence of the varicocele after the procedure. When this does occur, it occurs severals months to years after the initial treatment. About 10% of patients may experience recurrence. These results are less than those achieved with more invasive surgical techniques. Varicocele embolisation has been performed for over 20 years and has an excellent long-term safety record. Its safety and effectiveness has been shown in very large trials.
Very rarely there is a risk of damage to the walls of the veins which can lead to back discomfort lasting 2 to 3 days.
Treatment options
Currently there are two options for treatment of a varicocoele; embolisation or surgery.
Varicocoele embolisation
This is a non-surgical, day case procedure which is performed by an interventional radiologist. By this procedure, the vein is blocked internally, therefore accomplishing what a urologist does surgically, but without the need for surgery in the scrotum.
Surgical treatment
This is performed by a urologist, usually under general anaesthesia or sedation. Then an incision is made into the skin above the scrotum. The offending veins are identified and tied off with sutures. Recovery time is often two to three weeks. A keyhole operation is also possible using a laparoscope as is used for other common operations like gall bladder removal.
Advantages of varicocoele embolisation over surgery
- No surgical incision or sutures.
- As effective as surgery.
- Day case procedure with no overnight stay.
- Short recovery period of one to two days.
- Hardly any complications. Infection has not been reported.
- If a patient has varicocoeles on both sides, both can be treated at the same time.
What happens after the procedure?
Depending upon your general level of fitness and if you have required sedation and/or painkillers, you will observed in the recovery area of the Radiology department for a variable length of time. If you are stable and deemed well enough to go home, you will be discharged. If it has been decided that you require longer in hospital to recuperate from the procedure, you will be transferred back to the ward.
Nursing staff will be carrying out routine observations such as measurements of your blood pressure and pulse in order to ensure you remain stable. The area that has been used for the introduction of the needle will also be examined to make sure there is no bleeding.
Once you have been discharged home, it is important that you avoid any heavy lifting for 2 to 3 days after the procedure. It is also best to keep the skin site of the incision dry for 24 hours.
A follow-up appointment to see the Urologist who referred you to the Interventional Radiologist will be made, usually after an interval of at least 2 months after the procedure has been carried out.
You may not notice any appreciable difference to the varicocele for several months. It can take several months for the swelling to shrink fully, so don’t be alarmed if this is taking longer than expected.
How effective is Varicocoele embolisation?
Varicocoele embolisation is as effective as surgery for the treatment of varicocoeles as measured by improvement in pain, semen analysis and pregnancy rates. In one study pregnancy rates were as high as 60 percent. Another study showed that sperm parameters improved in 83percent compared to 63 percent for surgery. Patients who have had both procedures express a preference for embolisation.
References
- Keoghane SR, Kabala JE,Varicocoele Embolisation. Imaging, 13 (2001), 11-17
- Dewire DM, Thomas AJ Jr, Flak RM, et al. Clinical outcome and cost comparison of percutaneous embolization and surgical ligation of varicocele. J Androl 1994 15(suppl):38-42.
- Shlansky-Goldberg RD, VanArsdalen KN, Rutter, CM, Soulen MC, Haskal ZJ, Baum RA, Redd DC, Cope C, Pentecost MJ. Percutaneous varicocele embolization versus surgical ligation for the treatment of infertility: changes in seminal parameters and pregnancy outcomes. JVIR 1997;8:759-767.
- Feneley MR, Pal MK, Nockler IB, Hendry WF. Retrograde embolization and causes of failure in the primary treatment of varicocele. British Journal of Urology 1997;80:642-646.
- Nieschlag E, Behre M, Schlingheider A, Nashan D, Pohl J, Fischedick AR. Surgical ligation vs. angiographic embolization of the vena spermatica: a prospective randomized study for the treatment of varicocele-related infertility. Andrologia 1993;25:233-237.
- Lenk S, Fahlenkamp D, Gliech V, Lindeke A. Comparison of different methods of treating varicocele. J Androl 1994;15:34S-37S.
- Zuckerman AM, Mitchell SE, Venbrux AC, et al: Percutaneous varicocele occlusion: Long-term follow-up. J Vasc Interv Radiol 1994;5:315.
- Reyes BL, Trerotola SO, Venbrux AC, et al. Percutaneous embolotheraphy of adolescent varicocele: Results and long-term follow-up. J Vasc Interv Radiol 1994;5:131.
- Marsman JWP. Clinical versus subclinical varicocele: venographic findings and improvement of fertility after embolization. Radiology 1985;155:635-638.
Links to other sites
- Society of Interventional Radiologists, USA – Information on varicocoeles.
- http://www.sirweb.org/patients/varicoceles/ , and a printable fact sheet at http://www.sirweb.org/news/newsPDF/facts/Male_Infertility-Varicoceles_fact_sheet.pdf
- Varicocoeles.com – A US based website with information on varicocoeles.
- http://www.varicoceles.com/index.htm , including a monograph on varicocoeles at http://www.varicoceles.com/nonsurgical_varicocele_2006.pdf
