Patients
-
- Angiography
- Angioplasty and Stenting
- Aortic Aneurysms
- Biliary Drainage and Stenting
- Carotid Artery Stenting
- Central Venous Access
- Colonic Stenting
- Fibroids
- Gastrointestinal Haemorrhage
- Gastrostomy
- Hepatic Malignancies
- Kidney Tumour Ablation
- Minimally Invasive Treatments for Vascular Disease
- Nephrostomy
- Oesophageal Stents
- Pelvic Venous Congestion Syndrome
- Percutaneous Nephrolithotomy
- Prostate Artery Embolisation PAE
- Pulmonary Arteriovenous Malformations
- PAE Patient Information Leaflet
- Ureteric Stenting
- Varicoceles
- Varicose Veins
- Vascular Malformations
- Vertebral Compression Fractures
- Vertebroplasty and Kyphoplasty
Ureteric Stenting
Content by Dr Sivanathan Chandramohan and Dr Nadeem Butt, Gartnavel General Hospital, Glasgow.
Contents |
What is ureteric stenting?
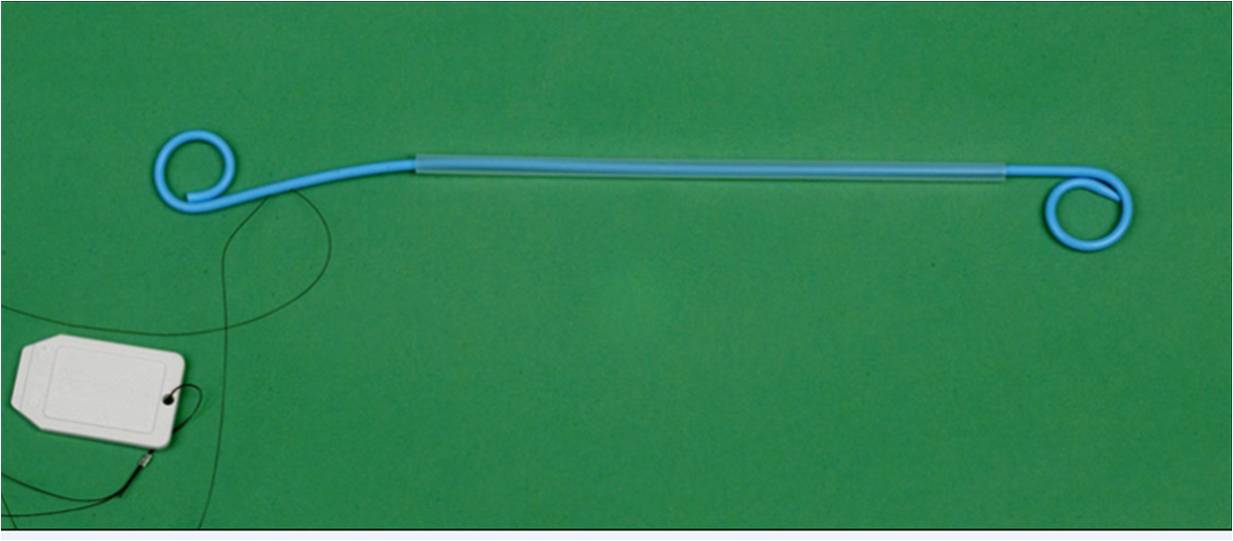
A ‘ureteral stent’ or ‘ureteric stent’ is a thin, hollow tube inserted into the ureter. Ureters are thin tube-like-organs which connect kidneys to the urinary bladder, to allow urine flow from the kidney. The stent is longer than the actual ureter and tube-ends are usually coiled. These coiled ends stay in the kidney on one side, and bladder on the other side, so as to minimise chances of its displacement. The length of the stents used in an adult patients varies between 24 to 30 cm. Stents come in differing diameters or gauges, to fit different sized ureters. Stents also contain small openings in their walls towards the ends, known as ‘fenestrations’. These fenestrations aid in the passage of urine.
Why do I need a ureteric stenting?
Sometimes, ureters can be blocked in many causes.
- It can be blocked within ureter. Blockage such as a stone can hinder the urine flow from kidneys to bladder.
- Some disease process such as infection, scar or tumour in the wall of ureter can obstruct the lumen of ureter.
- In other cases, any mass or swelling in side abdomen/pelvis can compress the ureter from outside.
- During few urological operations, ureters can be damaged. Such damages can leave scars behind which compromises urine flow. After such procedure related injury, stents can be left in ureter to avoid potential obstruction due to scar tissue.
Ureteric stent effectively treats these problems. It is a firm tube which keeps the ureters patent and allows urine flow ‘through the stent’ as well as ‘around it’.(1)
How is it done?
Ureteric stenting can be done in two ways:
- It can be done through the kidneys via a nephrostomy (an artificial opening made from the kidneys out to the skin.)
If you need a nephrostomy tube as well as ureteric stenting, your doctor may do both procedures at the same time. It is done by initially performing the nephrostomy and then using the nephrostomy to insert the stent into the ureters. This process is usually done in a radiology department under Ultrasound and x-ray guidance. General anaesthesia is usually not required for this and the procedure can be performed using sedation.
- It can also be done through the urinary bladder using a camera called a cystoscope or ureteroscope. Your doctor will pass a camera through the water passage and will access the urinary bladder. Once in the bladder, the lower opening of ureters can be seen through which the stent can be passed upwards to the kidney. It is usually done under general anaesthetic and using x-ray guidance in an operation theatre.
How long do the stents stay in my body?
It depends on the original cause of the disease process. Indwelling times may range from a few days for relief of ‘ureteral oedema’ (or you can call it swelling), to the duration of the patient’s life for maintenance of ureteral patency in obstruction from neighbouring cancer. Regardless of the stent composition, manufacturers usually recommend exchange of stents at 3 to 6 month intervals, and studies have shown that the prevalence of complications increases with longer indwelling times Your consultant will be able to advise you on this.(2)
Is there any alternative?
Ureteric stents allow the passage of urine along the natural route. However, if you do not prefer this, a nephrostomy can be an alternate. However nephrostomy drains urine from the kidneys through the skin and usually a bag is attached to the skin.
Surgical intervention can sometimes be done to avoid nephrostomy or ureteric stenting.
What can go wrong?
Irritative bladder symptoms remain the most common problem post stenting. You may find a change in frequency and volume of micturition.
Pain is another commonly encountered problem in ureteric stents. Although a large number of patients do not feel any pain due to stent placement, few patients, however, feel mild discomfort in the loin or supra-pubic region. Discomfort is often related to urination. Occasionally, it can be significant pain warranting removal of the stents.
Urinary tract infection: Stents like any other foreign material inside human body can cause infection and inflammation. Sometimes, infection is introduced at the time of stent placement and all patients are given antibiotic prophylaxis to avoid such cases.
If you think that you might have a urinary tract infection at time of procedure, please inform your doctor. Stenting in active infection is usually delayed until infection has resolved.
Malposition: Malposition of a stent is defined as an incorrect position during initial placement. Stents are usually carefully selected to match the length of ureters. An inappropriately sized stent can contribute to significant problems towards malposition and usually irritative bladder symptoms.
Migration: can be upwards to the kidney or downwards to the bladder. It is usually avoided by added loops to end of stent. These loops help anchoring the stent at the two ends.
Inadequate relief of obstruction: Blockade of a stent lumen may occur at any time following insertion into the urinary tract. Short-term luminal obstruction, occurring within hours to days of insertion, may result from blood in urine which is related to the technique or from increased urine viscosity and debris associated with insertion in an infected system.
Encrustation: Stent material is designed to be ‘inert’ or ‘non-reactive’ in the human body. This is aimed to minimise any reaction within the body against a foreign material present. However, in reality, none of the stents are inert within the urinary tract. The presence of the stent provides a framework for deposition of urine constituents. Over time, this will occur with any stent. To prevent encrustation, dilution of the urine with high fluid intake and aggressive treatment of any urinary tract infection should be undertaken. Prevention of encrustation and possible stent occlusion is also one of the major indications for regular exchange of ureteral stents where these are needed for longer periods of time. Regular exchange in such cases is always recommended by the manufacturer. Heparin coating is sometimes used on stents to avoid encrustations.(4)
Stent fracture: Urine is a hostile environment. Most fractures occur at fenestration sites, but the fenestrations are thought to be an integral component for optimizing flow via the stent. Encrustation is also likely to play a role in stent fragmentation. These complications are more frequent in long indwelling stents.
Ureteral erosion: A feared but rare complication of ureteral stent placement is erosion of the stent into adjacent structures, especially the arterial system.
Forgotten stent: Urinary environment and the stent placed within it are not stable for long periods of time. The prevalence of all consequences and complications increases the longer a stent remains in place. If you have a stent for long period of time (more than 3-6 months), it may be worthwhile to remind your doctor about this.
After you have stenting?
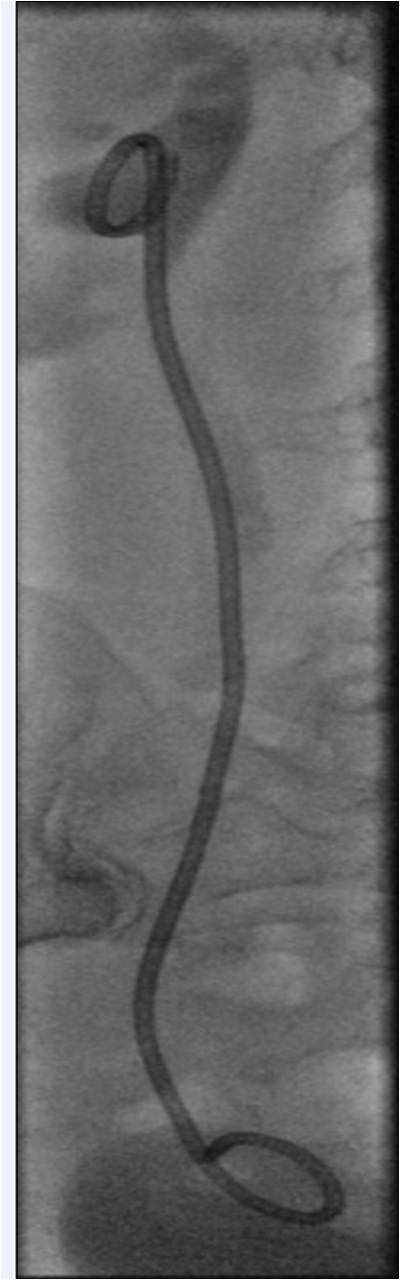
Stents can be seen on ultrasound scan and x-rays which can be done to evaluate the function and position of stents respectively.
You will get an x-ray of the abdomen to ensure that the stent is in place. These x-rays are some times performed again to see the effects of treatment or occasionally to rule our displacement of the stent.
References
1. High failure rate of indwelling ureteral stents in patients with extrinsic obstruction: experience at 2 institutions
Docimo SG, DeWolf WC.. J Urol 1989; 142:277-279.
2. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times.
El-Faqih SR, Shamsuddin AB, Chakrabarti A, et al.
J Urol 1991; 146:1487-1491
3. Complications of Ureteral Stent Placement
Raymond B. Dyer et al
September 2002 RadioGraphics, 22, 1005-1022.
4. "Heparin Coating on Ureteral Double J Stents Prevents Encrustations: An in Vivo Case Study.",
Cauda et al , J Endourol. 2008 22(3): 465–472,
Links (to other useful sites)
Complications: http://radiographics.rsna.org/content/22/5/1005.full#ref-19
