Patients
-
- Angiography
- Angioplasty and Stenting
- Aortic Aneurysms
- Biliary Drainage and Stenting
- Carotid Artery Stenting
- Central Venous Access
- Colonic Stenting
- Fibroids
- Gastrointestinal Haemorrhage
- Gastrostomy
- Hepatic Malignancies
- Kidney Tumour Ablation
- Minimally Invasive Treatments for Vascular Disease
- Nephrostomy
- Oesophageal Stents
- Pelvic Venous Congestion Syndrome
- Percutaneous Nephrolithotomy
- Prostate Artery Embolisation PAE
- Pulmonary Arteriovenous Malformations
- PAE Patient Information Leaflet
- Ureteric Stenting
- Varicoceles
- Varicose Veins
- Vascular Malformations
- Vertebral Compression Fractures
- Vertebroplasty and Kyphoplasty
Pelvic Venous Congestion Syndrome
Pelvic Venous Congestion Syndrome
Dr Shaheen Dixon1, Dr Charles Ross Tapping1, Dr Wei Chuen Liong2 and Dr Dinuke Warakaulle2
Departments of Radiology, 1John Radcliffe Hospital, Oxford and 2Stoke Mandeville Hospital, Aylesbury
What is Pelvic Venous Congestion Syndrome?
Pelvic venous congestion syndrome is also known as ovarian vein reflux. It is a cause of chronic pelvic pain in approximately 13-40% of women. Chronic pelvic pain is pain in the lower abdomen which has been present for more than 6 months. Pelvic congestion syndrome is therefore a painful condition often caused by dilatation of the ovarian and/or pelvic veins(rather like varicose veins but in the pelvis) . Varicose veins are commonly seen in the legs when the veins become less elastic and the valves that stop the blood from flowing backwards stop working. This causes the blood to pool, due to gravity, causing enlarged, bulging and knotty veins. This is also what happens to the pelvic veins in pelvic venous congestion syndrome (PVCS). This pressure results in the pain of PVCS and may also cause visible varicose veins around the vulva, vagina, inner thigh, sometimes the buttock and down the leg (s).
In order to understand what veins are dilated and why you get varicose veins in around the vulva/vagina and down the inner thigh it is important to know a little bit about the anatomy. The diagram below (Diagram 1) demonstrates the normal anatomy of the veins within the body.
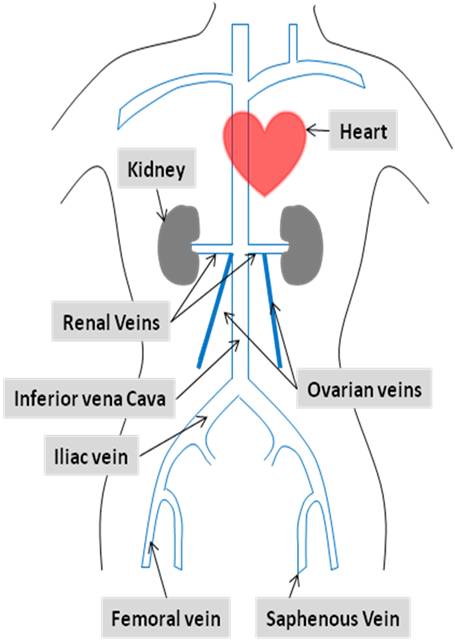 Diagram 1: Normalvenous anatomy: Normally the blood is pumped from the legs, through the veins in the pelvis and abdomen to the heart. The blood normally flows from the ovaries through the ovarian veins. The right ovarian vein joins the inferior vena cava and the left ovarian vein joins the left renal vein.
Diagram 1: Normalvenous anatomy: Normally the blood is pumped from the legs, through the veins in the pelvis and abdomen to the heart. The blood normally flows from the ovaries through the ovarian veins. The right ovarian vein joins the inferior vena cava and the left ovarian vein joins the left renal vein.
When the valves in the vein stop working or there is obstruction to the flow of the blood in the veins going back to the heart, the blood then flows backwards (i.e. the wrong way, away from the heart). This causes the varicose veins in the pelvis around the ovaries, vulva/vagina and down the inner thigh and legs, causing PVCS. Look at Diagram 2 and 3 which show what happens when the veins become abnormal.
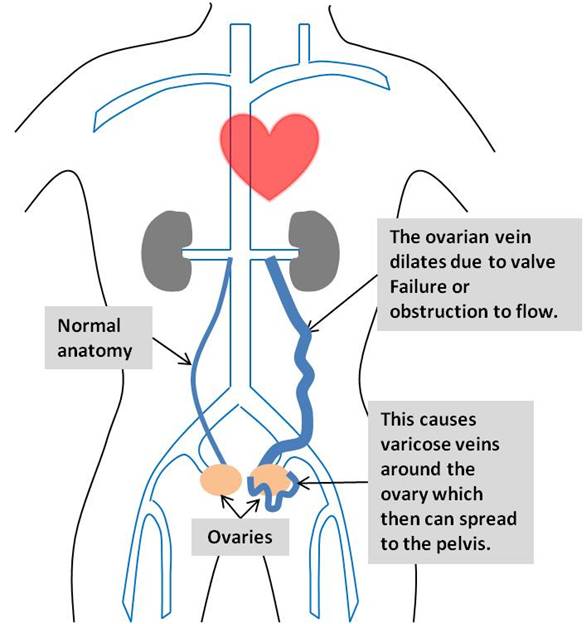 Diagram 2: Shows how the dilated vein looks and causes the varicose veins around the ovary because the valves don’t work. Blood flow is in the wrong direction, pooling in the veins and causing them to enlarge.
Diagram 2: Shows how the dilated vein looks and causes the varicose veins around the ovary because the valves don’t work. Blood flow is in the wrong direction, pooling in the veins and causing them to enlarge.
What are the causes of PVCS?
The cause of the dilated ovarian/pelvic veins in PVCS is poorly understood.PVCS most commonly occurs in young women , and usually in women who have had at least 2-3 children. During pregnancy the ovarian vein can be compressed by the enlarging womb or enlarged because of the increased blood flow. This is thought to affect the valves in the vein causing them to stop working and allowing the blood to flow backwards, contributing to PVCS.
There are other causes that may cause obstruction to the ovarian and pelvic veins leading to PVCS, which are much less common, and are the result of vein obstruction. PVCS may also be associated with polycystic ovaries.
The absence of the vein valves due abnormal development may be a contributing factor.
What are the symptoms and signs?
The symptoms of PVCS are due to the dilatation of the pelvic veins and because the blood is flowing the wrong way (i.e. backwards).
The varicose veins in the pelvis surround the ovary and can also push on the bladder and rectum. This can cause the following symptoms:
- Pelvic pain or aching around the pelvis and lower abdomen
- Dragging sensation or pain in the pelvis
- Feeling of fullness in the legs
- Worsening of stress incontinence
- Worsening in the symptoms associated with irritable bowel syndrome
Pain is usually commonest symptom and present for over 6 months duration. The pain is usually on one side but can affect both sides. The pain is worse on standing, lifting, when you are tired, during pregnancy and during or after sexual intercourse. The veins are also affected by the menstrual cycle/hormones and therefore the pain can increase during the time of menstruation. The pain usually is improved by lying down.
However, not every woman with pelvic vein reflux will get symptoms, and many only do following pregnancy. This is because after pregnancy, the veins can dilate more because of the compression from the womb. This then causes the varicose veins in the vagina/vulva to form (Diagram 3). The varicose veins can decrease after pregnancy, but may deteriorate over time.
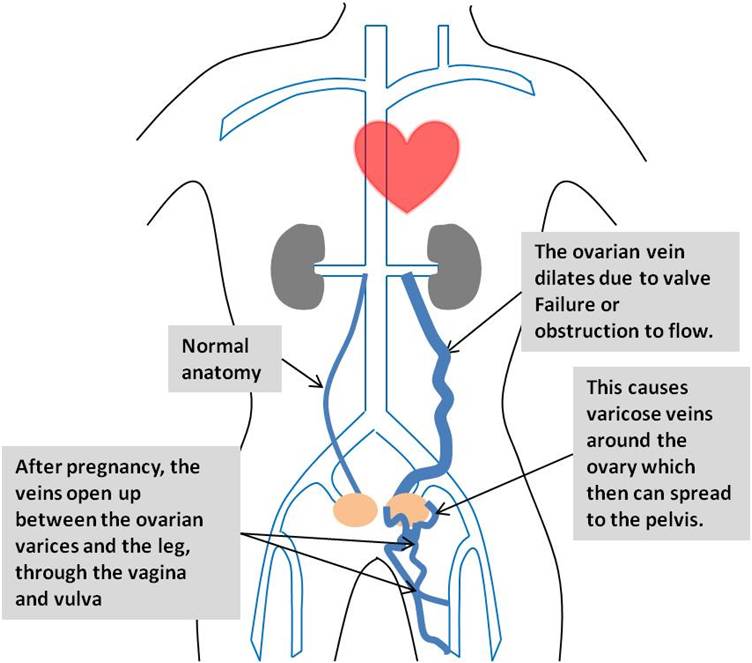
Diagram 3:Demonstrates the spread of the varicose veins down the medial aspect of the inner thigh. This usually occurs following pregnancy or if left untreated.
How is it diagnosed?
The first way to diagnose PVCS is by typical symptoms and if visible varicose veins are found on examination. Many women have a history of varicose veins around their vulva during their pregnancy. On examination you can seen these veins around the vulva, and they may extend down the inner thigh. On the inner thigh there is a muscle tendon along which the dilated veins are felt and seen. If the veins lie behind this tendon and or run behind the leg it is most likely they are dilated caused by reflux from the ovarian and/or pelvic veins.
Ultrasound examination may be useful (US). This imaging test uses sound waves to detect the abnormal veins. It is good at showing the blood flow through the veins and is non-invasive. However, sometimes the veins in the pelvis are difficult to see through the abdomen, therefore a special ultrasound where a small probe is placed into the vagina to see the veins, called a transvaginal ultrasound may be required.
The diagnosis may still require further investigation through non-invasive imaging with magnetic resonance imaging (MRI) and computed tomography (CT). This allows us to see where the varicose veins are coming from so that we can plan and do the appropriate treatment. Usually it is the ovarian veins that cause the varicose veins, but other pelvic veins can also be responsible.
Pelvic venography
Although US, CT and MRI may be initially used, pelvic venography is still used to diagnose PVCS and assess the anatomy before treatment is considered. This can be done at the same time as ovarian vein/pelvic vein treatment (embolisation) or as a separate procedure if the treatment options need further consideration. This is a more invasive test, but is a simple and safe diagnostic procedure. It is done by injecting dye (contrast) that can be seen on the x-ray machine (fluoroscopic machine) through a small tube (catheter) placed in the vein at the groin (the common femoral vein) or neck (internal jugular vein) under local anaesthetic. A catheter is placed in the ovarian and pelvic veins, contrast is then injected and the images seen on the fluoroscopic machine give a picture of the anatomy. It allows your doctor to see the abnormal veins. After the images have been taken, the tube is removed, and a little pressure is placed over the small cut in the groin or neck to stop any bleeding. You can then go home 1-4 hours later.
What are the treatment options?
As a first line, or if you feel that you do not want to under go a procedure, there are a few medical drug treatments (medroxyprogesterone acetate or more recently, goserelin), which has been shown to be effective in approximately 75% of women in reducing pain and the size of the varicose veins.
The usual treatment is percutaneous transcatheter pelvic vein embolisation. This is a minimally invasive treatment that is safe and can be done as a day-case. You come in for the procedure in the morning and can leave a few hours later the same day. In most cases it is the ovarian vein that is the cause of the varicose veins. However other pelvic veins such as veins called the internal iliac vein, internal pudendal vein, obturator vein and ischial veins may also be responsible and need treating as well.
Other treatment options are open or laparoscopic surgery to tie the culprit veins. Both these procedures are more invasive than ovarian vein embolisation and require a general anaesthetic and a longer recovery period.
How do I prepare for the Pelvic Vein Embolisation?
How do I prepare for the Pelvic Vein Embolisation?
- If you are taking warfarin, you will need to have this altered. Your doctor will advise you on the details before the procedure..
- Make sure that you take a list of all medications (including herbal medications) and mention any allergies you may have especially to iodine (as the x-ray dye, known as contrast, contains iodine).
- It is important to inform us of any recent illness, medical conditions or if there is any possibility that you are pregnant. The pelvic venography and pelvic vein embolisation procedures require x-rays which would expose the foetus to radiation if you were pregnant.
- You should wear comfortable clothing. You will be given a gown to wear during the procedure.
How is Pelvic Vein Embolisation performed?
Pelvic vein embolisation is a minimally invasive procedure performed by a specially trained interventional radiologist in the interventional radiology suite, usually within the x-ray (radiology) department. You will be positioned on a radiographic table with an x-ray machine and television-like monitor (which is suspended over the table) around you. This x-ray tube known as a fluoroscopy machine allows the x-ray images that are taken to be converted into video images so the interventional radiologist can watch and guide the progress of the procedure.
You will lie on your back during the procedure and will have a cannula (a small tube placed either in the back of your hand or at the elbow) to allow us to give any medication or fluid intravenously if required. You will also be connected to equipment to monitor your heart beat and blood pressure.
During this procedure, the interventional radiologist inserts a tube (catheter, a long thin plastic tube, usually around 2 mm in diameter into a vein). This is commonly done using a vein at either your groin or neck. This is done by a small nick in the skin. Local anaesthetic similar to that used at the dentist is used to numb the skin before the nick is made. You will feel a slight pin prick when the local anaesthetic is injected. You may feel slight pressure when the catheter is inserted but no serious discomfort.
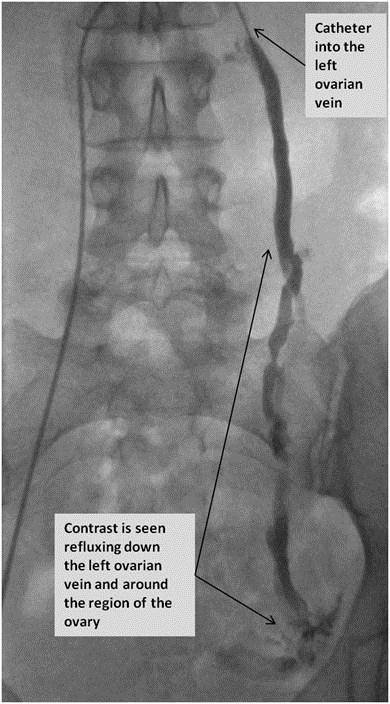
Using x-ray image guidance and contrast material to see the blood vessels, the catheter is then directed into the ovarian and/or pelvic vein(s) to see if there is any abnormaility, Diagram 4. As the contrast is injected into the veins and passes through your body, you may experience a warm, flushing feeling. This is norm
 |
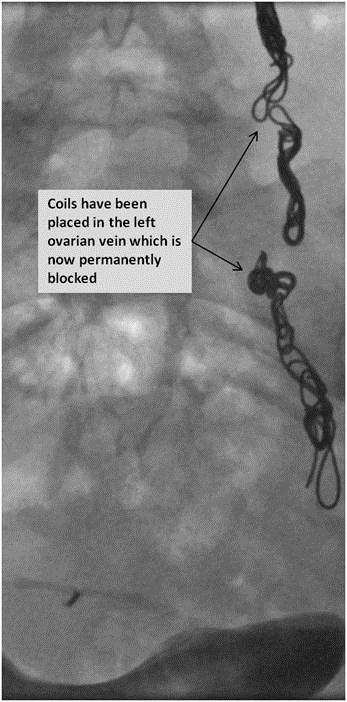 |
Diagram 4:(A)The catheter is seen within the left ovarian vein. Contrast (X-ray dye) is seen refluxing down the left ovarian vein. (B)This has been successfully embolised (permanently blocked) with coils. |
| A | B |
If an abnormality is shown, the same catheter can be used for treatment (Diagram 4). This is when the vein is sealed and blocked using synthetic material or medication called embolic agents. This is pushed out through the catheter to the treatment site. For the embolisation to be successful without injuring any normal tissue, the catheter needs to be placed in a precise position. This allows the embolic material to be delivered in only the abnormal vessels. However in a small percentage of cases, the procedure is not technically possible and the catheter cannot be positioned appropriately. If this occurs then another approach may be required. For example if the skin nick is done at the groin, another skin nick may be needed at the neck to approach the vein from a different position.
There are several embolic agents that the interventional radiologist may use depending on the size of the blood vessel and how much they need to treat. Many of these embolic agents have been used for over 20 years and are safe and effective.
The list of embolic agents that the radiologist may use are listed below:
- Coils – These are made of different metals including stainless steel or platinum. They come in various sizes and can block the larger vessels.
- Liquid sclerosing agents – These close up the veins by causing them to clot.
- Liquid glue – Similar to the liquid sclerosing agents, this is inserted into the vein where is hardens to block the vein.
At the end of the procedure the catheter is removed and pressure is applied to the area to stop any bleeding. The skin nick is small and no sutures are needed.
The length of the procedure is variable depending on the complexity of the condition. Typically it can take between 30 and 90 minutes. In a small number of patients, a repeat procedure may be needed to block all the culprit veins. This occurs when other pelvic veins beside the ovarian veins are abnormal (Diagram 5). However this is now very rare and most patients only require one embolisation procedure.
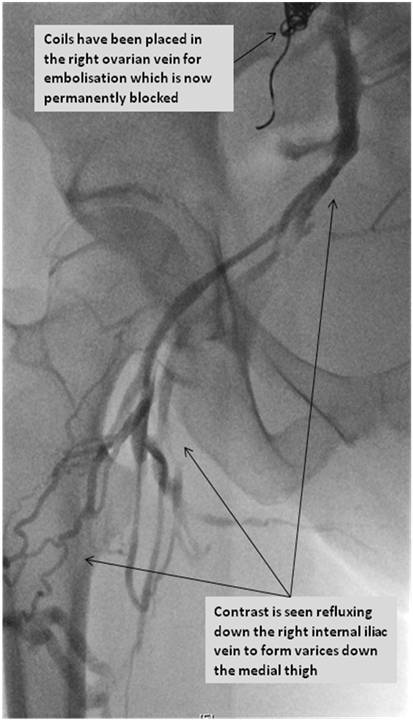 |
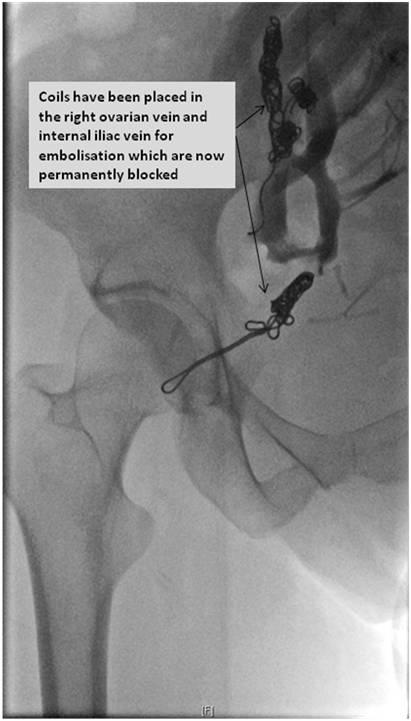 |
Diagram 5:(A)The picture shows that the ovarian vein has been blocked, but there are pelvic and medial thigh varicose veins. These are coming from the internal iliac vein on this side. (B) Demonstrates embolisation of the right internal iliac vein. |
| A | B |
What are the benefits and risks of the Pelvic Vein Embolisation?
Benefits
- Pelvic vein/ovarian vein embolisation has been shown to be a safe procedure with relief of the symptoms of pain, and improvement in the appearances of the varicose veins.
- Embolization is a highly effective way of blocking the vessel.
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
- Embolization is much less invasive than conventional open surgery. As a result, there are fewer complications and the hospital stay is relatively brief - typically this is done as a day case. Blood loss is less than with traditional surgical treatment, and there is no obvious surgical incision.
- A majority of women (up to 85%) find they have an improvement within 2 weeks of the procedure.
Risks
- There is a very slight risk of an allergic reaction if contrast is injected.
- There is a very small risk of infection after embolization
- Any procedure that involves placement of a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel (called ovarian vein thrombophlebitis), bruising or bleeding at the puncture site.
- There is a small chance that an embolic agent can lodge or migrate in the wrong place and deprive normal tissue of its oxygen supply (this is called non-target embolisation and occurs very uncommonly)
- Recurrence of the varicose veins can occur in up to 10%.
- Radiation exposure to the ovaries. However, there has been no evidence that fertility or periods are affected by the procedure.
What happens after the procedure?
Your heart rate and blood pressure will be monitored.
Some patients experience mild pain or discomfort following the procedure which can be controlled by simple medication given by the mouth or through your cannula, intravenously.
Following the procedure, bed rest is required for a short time and most people leave the hospital within 4 hours of the procedure. If you experience considerable pain, you may have to stay in hospital longer.
Once discharged, you are able to resume your normal activities within a few days. Driving should be avoided for 1 week, or longer if groin discomfort should persist (which is very rare).
Your interventional radiologist may recommend a follow-up scan and visit after your procedure or treatment is complete. This is to check whether the procedure has been a success, and also allows you to discuss any changes or side-effects you have experienced from the treatment. The visible varicose veins may require local treatment, similar to other leg varicose veins.
By stopping the blood refluxing (flowing the wrong way), the pelvic varicose veins should gradually shrink away over a few weeks. If you have any vulval varicose veins, these should also gradually shrink. Now that the main ovarian and pelvic veins have been embolised, if you also have any lower leg varices, these can be treated with a reduced chance of them coming back in the future (which they have a high chance of coming back if you did not have the pelvic vein embolisation). Any symptoms that you have been having related to the varicose veins in the pelvis should also slowly improve.
References
- Bittles MA, Hoffer EK. Gonadal vein embolization: treatment of varicocele and pelvic congestion syndrome. Semin Intervent Radiol. 2008;25(3):261-70.
- Ganesh A, Upponi S, Hon LQ, et al. Chronic pelvic pain due to pelvic congestion syndrome: the orle of diagnostic and interventional radiology. Cardiovasc Intervent Radiol. 2007;30:1105-11.
- Ignacio EA, Dua R, Sarin S, et al. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol. 2008;25:361-8.
- Ratnam LA, Mark P, Holdstock JM, et al. Pelvic vein embolisation in the management of varicose veins. Cardiovasc Intervent Radiol. 2008;31:1159-64.
Useful Links
http://www.radiologyinfo.org/en/info.cfm?pg=ovariveinembol
http://www.veindirectory.org/content/pelvic-congestion-syndrome.asp
http://www.ecommunity.com/interrad/index.aspx?pg=6946
