Patients
-
- Angiography
- Angioplasty and Stenting
- Aortic Aneurysms
- Biliary Drainage and Stenting
- Carotid Artery Stenting
- Central Venous Access
- Colonic Stenting
- Fibroids
- Gastrointestinal Haemorrhage
- Gastrostomy
- Hepatic Malignancies
- Kidney Tumour Ablation
- Minimally Invasive Treatments for Vascular Disease
- Nephrostomy
- Oesophageal Stents
- Pelvic Venous Congestion Syndrome
- Percutaneous Nephrolithotomy
- Prostate Artery Embolisation PAE
- Pulmonary Arteriovenous Malformations
- PAE Patient Information Leaflet
- Ureteric Stenting
- Varicoceles
- Varicose Veins
- Vascular Malformations
- Vertebral Compression Fractures
- Vertebroplasty and Kyphoplasty
Biliary Drainage and Stenting
Dr Andrew Hatrick and Dr Joo-Young Chun
Contents |
What is percutaneous biliary drainage?
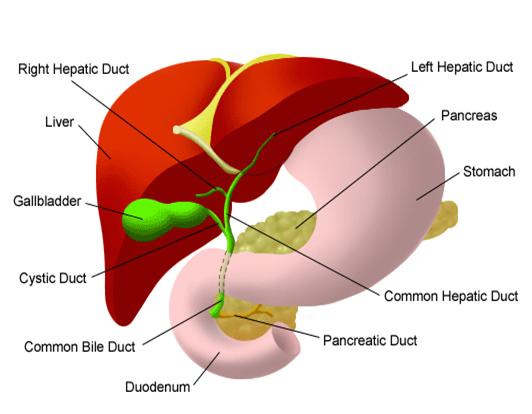
Percutaneous transhepatic biliary drainage is a procedure where a small, flexible, plastic tube is placed through the skin into the liver in order to drain an obstructed bile duct system.The liver produces bile which aids digestion of fats. The bile flows through a series of small tubes (ducts) that drain into one large duct called the common bile duct, which then empties into the duodenum, the first part of the small bowel after the stomach. Bile is also stored in the gallbladder.
If the bile duct becomes blocked, the bile cannot drain normally and backs up in the liver. Signs of blocked bile ducts include jaundice (yellowing of the skin), dark urine, light stools, itching, nausea and poor appetite. This is a potentially serious condition that needs to be treated. It is possible to relieve the obstruction by inserting a fine plastic drainage tube (catheter) through the skin (percutaneous) into the obstructed bile duct, past the obstruction and into the duodenum.
T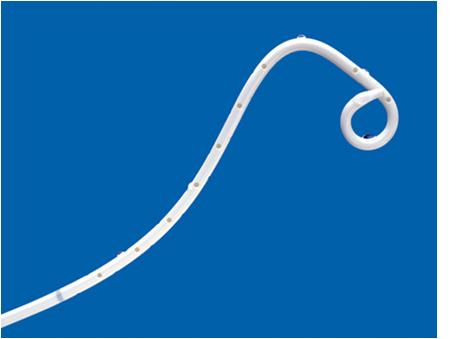 his relieves the congestion in the blocked duct by allowing the bile to drain externally into a collecting bag as well as draining internally in the normal way.
his relieves the congestion in the blocked duct by allowing the bile to drain externally into a collecting bag as well as draining internally in the normal way.
(A biliary drain)
What is biliary stenting?
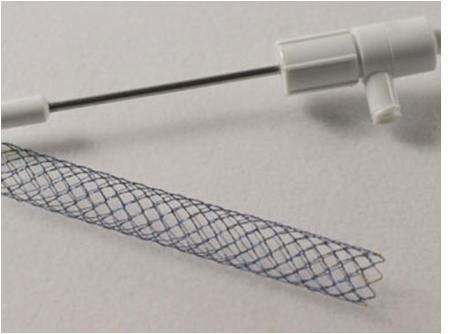
Sometimes the biliary drainage procedure may be extended with the placement of a permanent plastic or metal stent across the site of the bile duct blockage. Stents are usually inserted a few days after the initial drainage procedure and they keep the narrowed duct open without the need for a catheter.
Stenting may be preceded or followed by biliary dilatation, which involves dilating a segment of bile duct with a balloon to open up the stricture.
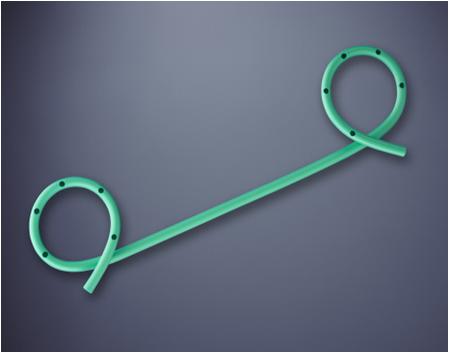
(A plastic biliary stent)
(A metal biliary stent)
What are the indications for percutaneous biliary drainage +/- stenting?
The most common indication for biliary drainage is blockage or narrowing (stricture) of the bile ducts. There are several conditions that may cause this including:
- Gallstones – in the gallbladder or within the bile ducts
- Inflammation of the pancreas (pancreatitis)
- Inflammation of the bile ducts (sclerosing cholangitis)
- Tumours of the pancreas, gallbladder, bile duct, liver
- Enlarged lymph nodes in the region of the pancreas and liver due to various types of tumours
- Injury to bile ducts during surgery
- Infection
Biliary drainage relieves obstruction by providing an alternative pathway to exit the liver.
Biliary drainage may also be necessary if a hole develops in the bile duct, resulting in leakage of bile into the abdominal cavity. This leak may cause severe pain and infection. Biliary drainage stops the leak and helps the hole in the bile duct to heal.
Biliary drainage may be necessary in preparation for surgery or other procedure on the bile ducts, such as removal of a bile duct stone or tumour.
Who will perform the procedure and where will it take place?
 The procedure is performed by interventional radiologists. They are doctors specializing in minimally invasive treatments using image guidance. Interventional radiologists are trained to use diagnostic imaging equipment, such as x-ray and ultrasound, to guide various instruments during a procedure. The procedure will take place in the Interventional Radiology Department in a room especially adapted with x-ray and ultrasound equipment.
The procedure is performed by interventional radiologists. They are doctors specializing in minimally invasive treatments using image guidance. Interventional radiologists are trained to use diagnostic imaging equipment, such as x-ray and ultrasound, to guide various instruments during a procedure. The procedure will take place in the Interventional Radiology Department in a room especially adapted with x-ray and ultrasound equipment.
(A typical interventional radiology suite)
What are the risks of the procedure?
Although biliary drainage is a relatively safe technique, there are potential risks as with any procedure. Occasionally, it may not be possible to place the drain in the bile duct, in which case surgery may be required to relieve the blockage. Sometimes the bile may leak around the catheter and form a collection in the abdomen that can cause pain and may require drainage. Occasionally, the procedure can cause a blood infection (septicaemia) but prophylactic antibiotics are given to reduce this risk. Occasionally, bleeding may be a problem that requires a blood transfusion. Rarely, bleeding can be more severe and an embolisation procedure or surgical operation may be necessary.
With regards to biliary stents, they may be misplaced at the time of the procedure or may migrate following the procedure. These can be rectified by placement of a second stent in the correct place.
What happens after the procedure?
You will be taken back to your ward where your blood pressure, pulse rate, oxygen levels and temperature are monitored regularly. You will be on best rest for a few hours until you have recovered. It is important to take care of the drainage bag so that the catheter does not get pulled out. The nurses will empty the drainage bag at regular intervals and record the drainage output. If you are discharged with the catheter and bag in place, the nursing staff will teach you how to care for the catheter at home, such as how to empty the bag and change the dressing.
